Categories
Recommended Posts

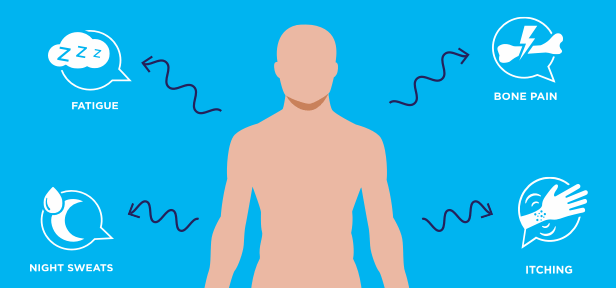
Focus on MF: 3 Ways to Stay Ahead of Your Symptoms
Author: Voices of MPN
Don't watch and wait for your symptoms to get worse. This year for Blood Cancer Awareness Month, we're showing you easy ways you can take an active role in your care.
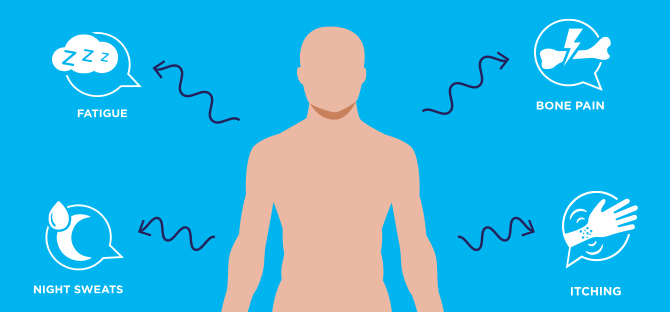
On Rare Disease Day 2025, Shine a Spotlight on MPN Symptoms
Author: Voices of MPN
On the last day of February, Rare Disease Day is observed globally to raise awareness for rare diseases and create a platform for those within the community.