Bob: What I Learned on My Journey With Myelofibrosis
Author: Bob W, Community Voice Champion
In the summer of 1983, I looked like any other graduate student at the University of Georgia. I happened to be a soccer player, and after a game one day, my left abdomen starting hurting. A lot.
After a few visits to local doctors, a hematologist looked at me and said, “You’re only 28. I had thought I would be telling you that you have something like mononucleosis. But you have primary myelofibrosis (MF).”
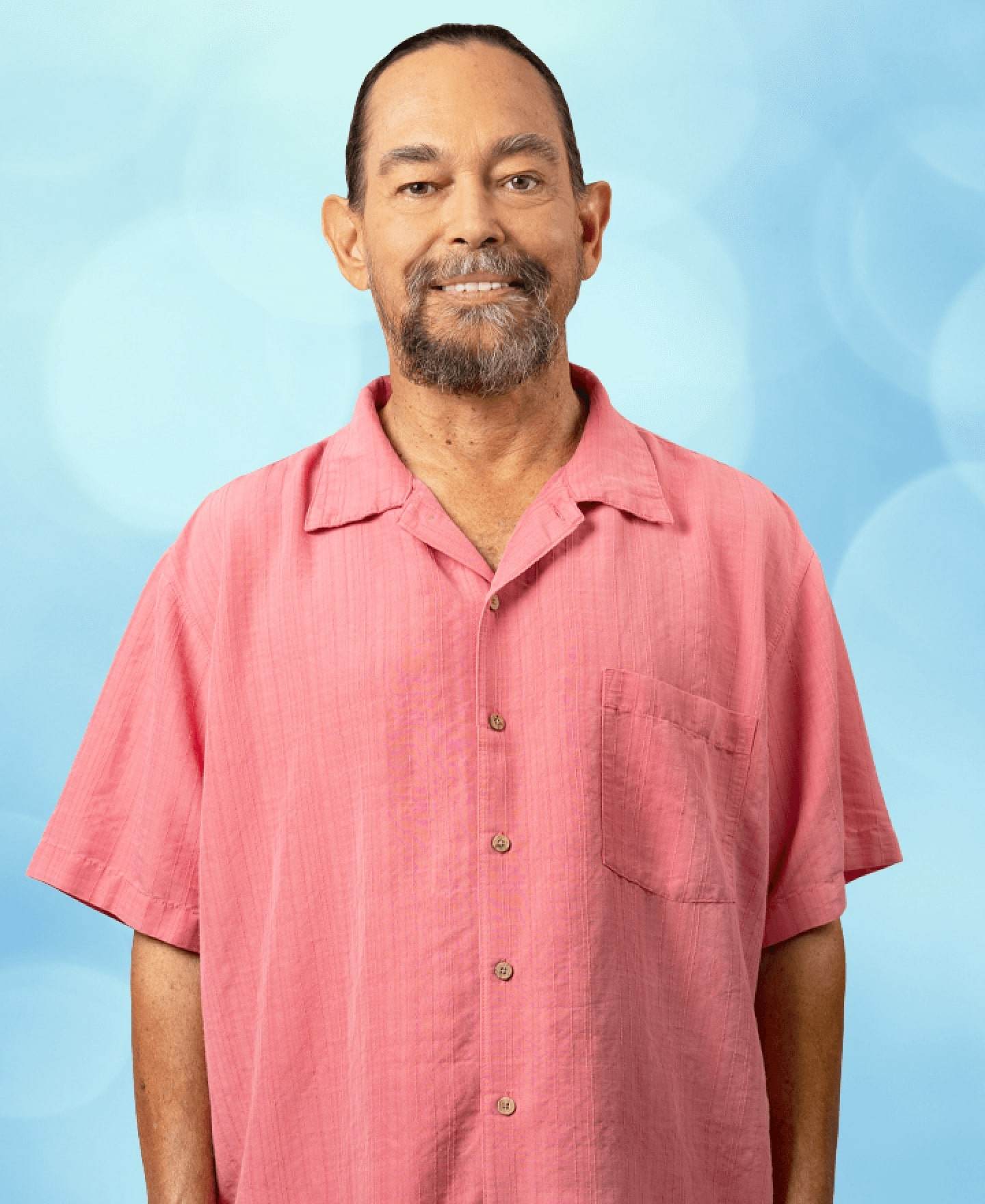
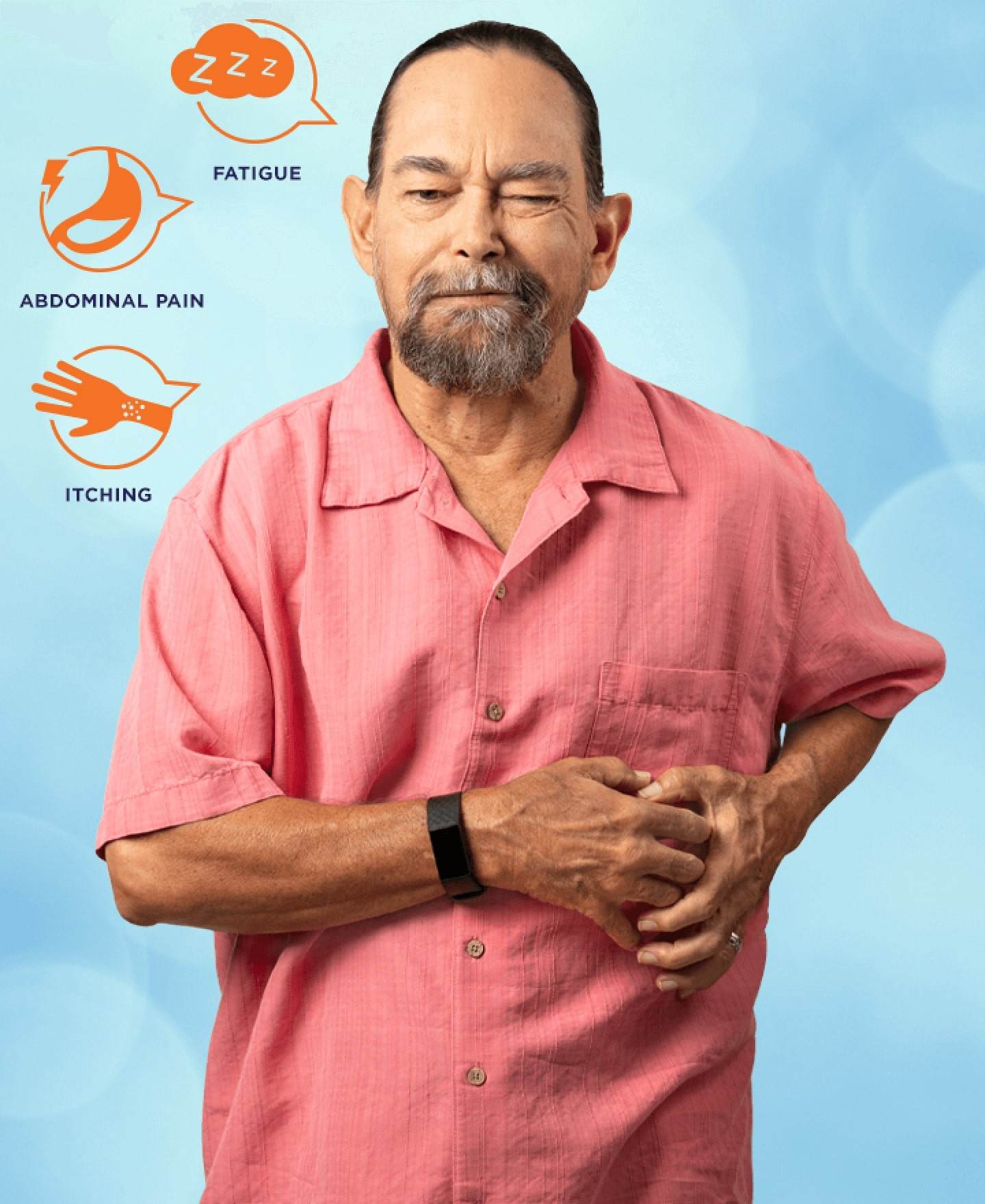
I was instantly confronted with the fact that how I looked on the outside—in this case, how the hematologist saw me—didn’t match how I felt on the inside. My abdomen hurt (because my spleen was enlarged) and I had brain fog. Those were the first symptoms of my journey with myelofibrosis.
As a soccer player, I was used to working through pain. I coped with my MF by pushing through it. I pushed through a lot of stuff that maybe I shouldn’t have. People didn’t realize I had myelofibrosis. Even today, my friends and family don’t fully understand my MF. In my case, it’s difficult to explain because I do look really healthy.
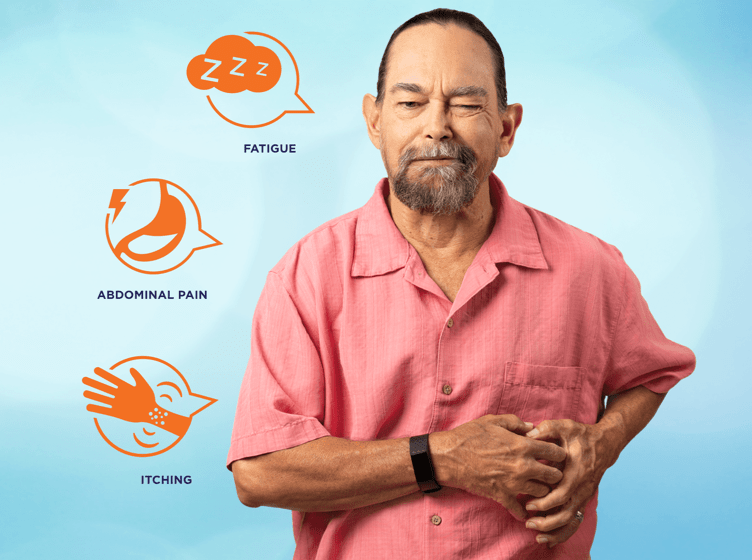
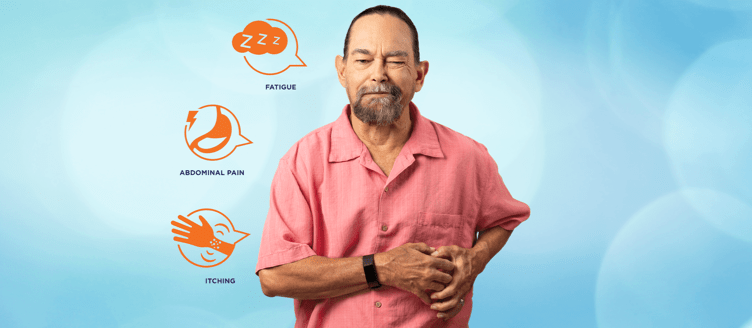
With my MF, I have gone through a range of symptoms that are not visible on the outside. I get full in my left abdomen. I have sharp pains there. My anemia sneaks up on me, and I feel internally exhausted.
Brain fog, which you also can’t see, impacted my job. I looked fine sitting at the computer, but I wasn’t connecting on all cylinders. Sometimes I don’t think as sharply as you might expect as when I’m on top of my game. All the while, though, I don’t look “sick.”
The other symptom I have is pruritus, intense itching. Sometimes it would distract my boss. It wasn’t until I looked into it that I realized that the itching was a symptom of MF. Unless you saw that I was itching a lot, my MF is not all that noticeable.
But I know it’s there and I have to do what I can to take care of myself. My wife and I eat healthy foods. I take a walk in the morning for about an hour, try to do yoga every day, and find the time for my stretching exercises. I go to bed at a regular time. For fun, I enjoy talking politics and stopping by the local coffee shops.
Education and support are important, too. I’m always online looking for different articles. I belong to two Facebook groups. When there are local MPN support meetings, I go to them. I meet other patients and talk with them about their journeys and what’s going on with them.
As I share my own journey, I’d want to change the way folks see MF. For people who have been newly diagnosed with MF—or any MPN—I’d tell them to take a deep breath and realize that you now need to be in charge of this. Of course, you and your doctor will work together during your journey, but you really need to step up and empower yourself.
The other thing I’d say about the way people see MF is that you’re not in a battle. However, you now have a new dance partner that you’re going to be dancing through life with. As in any good partner dance, leading and following is going to shift back and forth between you and the disease. So I suggest that the more you can flow with it and be optimistic, the easier a lot of things will be.
As Bob mentioned, it’s important to become your own advocate when living with an MPN. The MPN Tracker Tools can help you track your symptoms, blood counts, and procedures, so you can share how you’re feeling with your healthcare team.
This is Bob's personal journey with MF. Each MPN patient is different and their experience will be unique to them.
Related Articles


Barbara Reveals Hidden Struggles in a Film About the Impact of MPNs
Author: Voices of MPN
READ ARTICLE