Denise: Investing in a Positive MPN Perspective: My MPN Journey

Author: Denise T, Community Voice Champion
I have always been an active person. I’ve run marathons. I’ve cycled 250 miles. I’ve even achieved a black belt in karate. I’ve also been living with a myeloproliferative neoplasm (or MPN) for 39 years—although you wouldn’t know it by looking at me.
It all started during my senior year of college. I was on the women’s cross-country running team. I remember having a lot of trouble recovering from my workouts, although I didn’t understand why, at the time. It got so difficult that I ended up quitting the team before I even ran my first race. About 6 months later, I started getting migraines for the first time in my life. Looking back, I realize that my body was trying to tell me something. But back then, I didn’t know what it was saying.
About a year later, I was scheduled for a minor surgery. The routine pre-operative blood work revealed that my platelet count was 1.2 million. I was sent to a hematologist/oncologist for further testing, and a bone marrow biopsy confirmed that I had a rare, chronic blood cancer called essential thrombocythemia, or ET. That word—cancer—was much scarier back then. I didn’t know what it meant for me. I was told that the average life expectancy for someone with ET was about 10 years. But I was in my 20s, and I still had my entire life ahead of me. I decided in that moment that I was going to live it to the fullest.
At the time, I was pursuing a career in finance. It wasn’t the kind of environment where you could show any signs of weakness. So I pushed through it, and I kept quiet about my MPN, really only talking about it with my healthcare team.
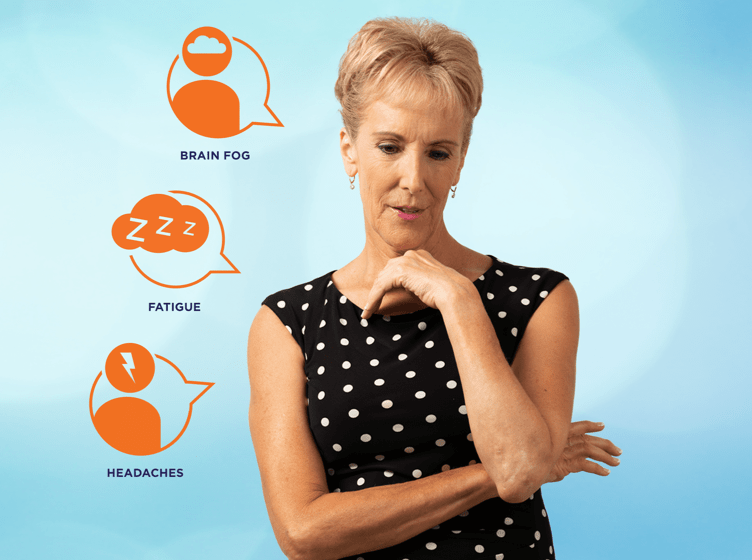
It was easy enough to hide my MPN symptoms. For example, no one could see when I felt dizzy or had brain fog. I looked healthy on the outside. In fact, even my doctors seemed to underestimate how I was feeling. One doctor said, “You look too healthy to be sick.” And another one ushered me out of an appointment once by saying, “Get outta here. I need to treat sick patients now.” I know they meant well, because I really did look fine. But it was frustrating, because my symptoms were real.
Between 1986 and 2013, I achieved a good deal of success. I had become the chief financial officer (CFO) of a global company in 1992 and continued in that role at various companies for over 25 years. During that time, new and more pronounced symptoms started. I experienced significant brain fog and fatigue. Eventually, my fatigue had gotten so bad that I sometimes couldn’t even get through a full day of work. I also started to suffer from bone pain and burning, itchy skin (pruritus) that would feel like it was on fire for 15 minutes after I showered.
I was already seeing my healthcare team on a monthly basis, but I decided to find an expert, an MPN specialist to learn what more I could do about it. I would encourage anyone affected by an MPN to see a top expert in the MPN field, who is up to date with the latest research, at least once. I was also doing my own research and attended several conferences so that I could make informed decisions about my own health.
Life was busy. In late 2017, things changed again. I was seeing my doctor regularly. I was still working full time, but managing my MPN became a second job. It took a lot of time and energy. I started experiencing overwhelming fatigue, dizziness, and trouble concentrating, which greatly impacted my work. Tests revealed that although my hemoglobin levels were in the normal range, there was significant fibrosis in my bone marrow. My MPN specialist diagnosed it as polycythemia vera with fibrosis.
By 2018, I knew that something had to give. Initially, I tried to take work head-on by making changes to my work schedule: starting work at 6am and scheduling important meetings early as I felt better in the morning, working some days at home, working shorter hours, and stopping international travel. But my body was shutting down, and I knew that I needed to listen to it. Later that year, I decided to go out on long-term disability. That was a tough choice, as I loved my career. However, I knew that I had to rest and address my health issues, and it made a difference.
Today, my healthcare team and I continue to look for new ways to help me live with my changing symptoms. I also continue to exercise. That really helps with the brain fog and improves my mental clarity. I also walk more than I ever did before. But I rest more, too. And I continue to see my doctors on a regular basis, including my MPN specialist.
I’m not giving up on the future as I know there are wonderful and fulfilling experiences in store for me. I encourage other MPN patients to live their fullest life within whatever constraints they have. Whether you’re someone who has just been diagnosed—or someone who has been living with an MPN for years—the most important things you can do are to stay positive, stay informed, make your own choices, and don’t look back. There is always new research coming out; new medical advances being made. Get yourself in your own comfort zone, whether by visiting websites, reading, getting second opinions, joining support groups, or just living life. And perhaps consider connecting with someone who, like you, is living with an MPN and understands what you are going through.
Find your own MPN specialist
Physician assistant Amber Essenmacher explains the potential benefits of consulting an MPN specialist.
This is Denise's personal journey with PV. Each MPN patient is different and their experience will be unique to them.
Related Articles

Susan: Living a Life Well-Lived: My Essential Thrombocythemia Journey
Author: Susan W, Community Voice Champion
READ ARTICLE