

What Is PV?
Polycythemia vera (polly-sigh-THEE-me-ah-VAIR-Ah), or PV, is a rare, chronic blood cancer where the bone marrow produces too many red blood cells. You may also have too many white blood cells and platelets (blood clotting cells) in your blood, but having too many red blood cells causes most of the problems associated with this condition. PV is part of a group of diseases called myeloproliferative neoplasms, or MPNs.
Too many red blood cells can cause the blood to thicken. Thicker blood doesn’t flow normally through arteries and veins. Increased blood thickness and decreased blood flow, as well as abnormalities in your platelets and white blood cells, may increase your risk of blood clots. Blood clots can cause a stroke, heart attack, or blockage of an artery in your lungs or in a vein deep within a muscle in your arms or legs.

What the EKG had, in fact, detected, was my heart struggling to push my abnormally thick blood through my body. —Matt W, PV Community Member
Can PV Transform Into Other Blood Diseases?
PV usually develops slowly. But as the symptoms get worse, they can take a toll on you and affect your daily life. In a very small number of people, PV leads to other blood diseases, such as myelofibrosis (MF) (a disease in which scar tissue develops in the bone marrow) or leukemia.
Learn more about what PV is or about the signs and symptoms.
Watch physician assistant and Medical Science Liaison (MSL) at Incyte Amber Essenmacher explain the association between blood counts and the risk of complications for people living with PV.
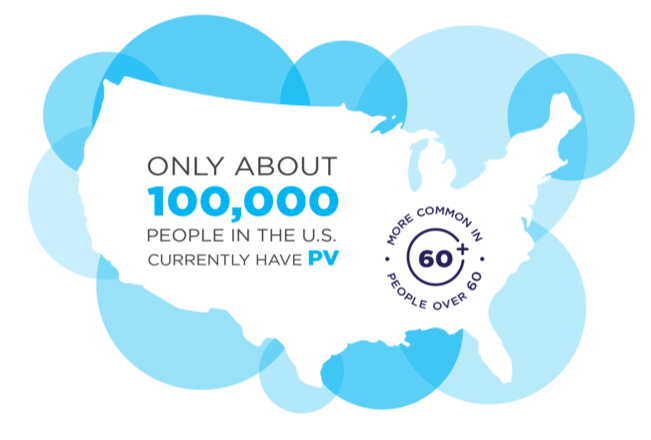
How Common Is PV?
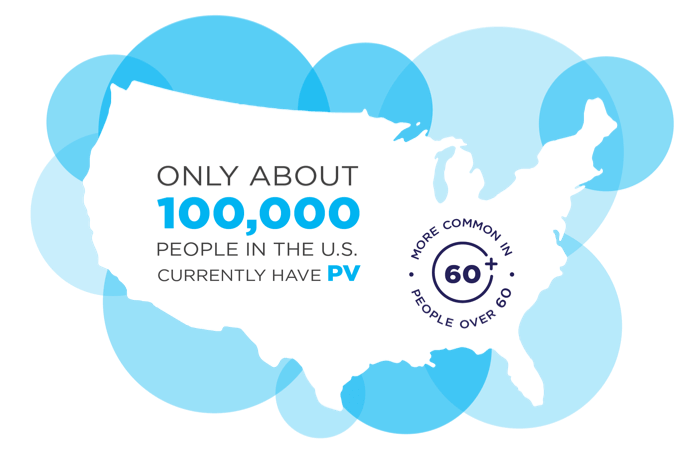
Approximately 100,000 people in the United States are living with this rare disease. PV can occur at any age, but it is more common in people over 60 years of age. It affects slightly more men than women.
Learn more about how PV is diagnosed.
How Is It Managed?
Management may include low-dose aspirin. Phlebotomy, a procedure that helps lower blood cell counts by removing blood from the body, may also be used. Patients who have difficulty with phlebotomy, who have an enlarged spleen, who experience severe PV-related symptoms, or who continue to have elevated blood counts may have other care management approaches, including but not limited to chemotherapy drugs.
View polycythemia vera educational materials.
What Is the Prognosis for People With PV?
There is no single, one-size-fits-all answer regarding the life expectancy associated with PV. Each individual journey is unique, and how PV may change over time will vary from person to person.
PV can often be effectively managed for a long period of time with ongoing medical supervision and an individualized management plan. The median survival for people with PV can be up to 20 years or longer, depending on the individual and his or her specific management approach. However, PV can worsen (progress), and in some cases, transform into myelofibrosis.
Your specific medical situation should be evaluated by your Healthcare Professional, who is the best source of information about life expectancy with PV.
Speak Up—and Spell Out How Your PV Makes You Feel
When you’re living with PV, you may find yourself saying that you’re fine—even when you might not be. But when you don’t speak up and share how you really feel, you may miss out on the opportunity to get the care and support that you need and deserve.
Remember, changes in your PV symptoms could be a sign that your PV is changing, too. So be sure to spell out how you really feel. Because fine is not enough.
View PV resources to help you take an active role in your care.
VIEW TRANSCRIPT 

“I work in healthcare, and I have patients that come in and have a hard time opening up.”
—Christine, diagnosed with PV
View More Stories About People With PV
Read articles written by—and for—the PV community